Male Urinary Incontinence Clamps for Mild to Severe Leakage Male urinary incontinence is a condition in which the patient has no control over their bladder.
Welcome to the futures of innovating product design at Medgo®. We are the most advanced wholesaler of natural products for men and women of all ages. Our quality products offer solutions in using: incontinence clamps, kegel weights, prostate massagers, hemorrhoid treatments, and weight loss. Medgo® was created in 2006 and has built an enterprise of independent distributors who have the same goals. Our mission is to collaborate with our loyal customers to provide solutions for real-life health problems. The vision at Medgo® is to provide superior products while placing the highest value on customer service.
We provide sensitive products that help both men and women who suffer from weight loss, hemorrhoids, prostate, and incontinence issues. These products are necessary items to have in your house and we understand the importance of being discreet. Our professional staff is trained to deal with customers on a human level. You should never have to feel ashamed to call and ask questions about a product that you need. Physical therapists and physicians recommend our products; therefore, a need for our products is necessary.
These products are designed to help individuals who struggle with sensitive health problems. They enhance your overall quality and provide a sustainable way to achieve a healthier life. When the inner parts of the body are damaged, professional inner body exercises are needed to restore muscles. When obesity is taken over your life and all other diet methods have failed, a powerful supplement is needed. Medgo® has been a trusted source for years, and we constantly drive innovative products to market.
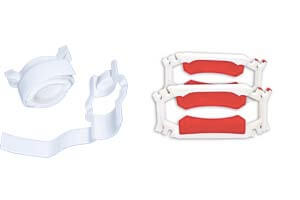
Kegel weights is an exercise system designed to strengthen the pelvic muscles. There are a lot of women who suffer from serious health and mental issues due to weak muscles. Weakened pelvic floor muscles can affect a woman’s sex life and they can also cause leakage. Our kegel weights exercise system is necessary to rebuild the vaginal canal and improve the quality of life for women. It is an exercising device that can be used along with kegel exercises to strengthen the correct muscles.

Peristal is the best hemorrhoid treatments on the market. It happens to be the world’s only and first hemorrhoid treatments device. It’s designed to work naturally with your own body’s inner muscles. The benefits of massaging hemorrhoids are to bring circulation back to the heart, therefore, reducing the size of the hemorrhoid. The Peristal is not an external device; it’s designed for internal use only. This product is excellent for toning kegel muscles and it is great for incontinence. It also provides a better long-term solution over traditional ointments that can be ineffective.

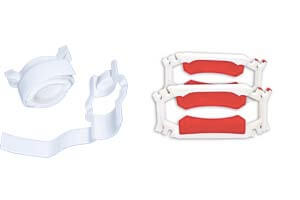
These Incontinence Clamps are the best device on the market that stops leakage in its tracks. It’s an effective penile clamp for those who have undergone radiation treatment, prostate surgery, and other health complications. This is an external device that can be clamped on the penis and applied to the urethra. It stops the embarrassing flow of urine and when wearing incontinence clamps, comfortable. These devices are made to be washable, and it allows the circulation of blood to flow normally.

Prostate Massagers is a hands-free massager that can be used in the privacy of your own home. This device focuses on the sphincter muscle while increasing circulation of the prostate gland. It increases sexual pleasure and is a very effective solution for therapeutic or medical applications. This device can help with chronic prostatitis, erectile dysfunction, and supports a wide range of conditions. The benefit of using the Prostate Massager is it can clear away excess fluid that is causing your discomfort.

These and other quality natural products are what drive Medgo®’s ambitions of providing solutions for all genders. All of our products are backed with a 100% money back guarantee. We offer discreet shipping & billing, secure shopping, secure checkouts with the best email and phone support available. Our customer service department is unmatched with real people that care about you! The importance of being able to help yourself in today’s world means everything. Medgo® is here to help assist you with “must have” products to improve your quality of life. Email us or pick up the phone and call one of our friendly representatives to get your order started immediately.
Male Urinary Incontinence Clamps for Mild to Severe Leakage Male urinary incontinence is a condition in which the patient has no control over their bladder.

Incontinence Pads and Pills Cause Damage Urinary incontinence is a condition that affects a significant number of people. It is prevalent among new mothers and

How to do Kegel Exercises For Men People often associate Kegel exercises with women only but Kegel exercises for men do exist. This exercise can

Do Kegel Balls Work? Kegel balls have been around for centuries. People use Kegal balls in their quest to strengthen pelvic floor muscles. Stronger pelvic
Vaginal Weights – Ultimate Weightlifting Guide To Pelvic Fitness Vaginal weights are essential for pelvic muscle exercises. After giving birth, women may suffer from stress

Kegel Weights Best Advanced Exercise System Kegel weights play an essential role in enhancing the results of Kegel exercises. However, there not very effective without
* 100% Discreet Shipping
* Secure Shopping
* Trusted for 12 Years
* No Catalogs Mailed to Your Home
* Real People That Care About You
Call: 941.445.6005
© COPYRIGHT 2006-2018 MEDGO ® LLC. ALL RIGHTS RESERVED.
Our Healthy products are not intended to diagnose, cure or prevent any disease.